Student with SOFTT-W tourniquet. Bleeding out can occur in less than five minutes. Tourniquets stop life-threatening hemorrhage fast. Students became proficient in rapid and proper application of tourniquets.
Emergency medical training should be part of the basic skill sets of every firearms owner. In fact, it should be part of the basic skill sets of everyone. The time to learn how to use a trauma kit is not when someone is bleeding out.
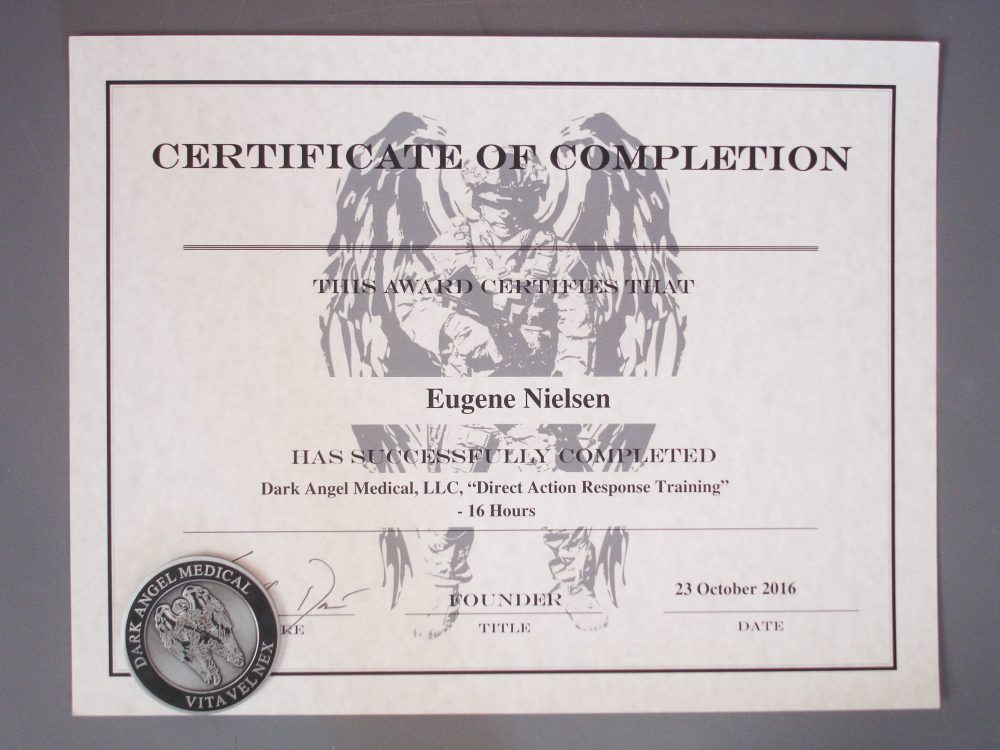
I recently had the opportunity to attend the Dark Angel Medical Direct Action Response Training (DART) hosted by Scottsdale Gun Club in Scottsdale, Arizona. Geared toward those with little to no medical training or background, the 16-hour, two-day course is designed to fill the niche between military self-aid/buddy-care training and civilian EMS training. The course provides the student with critical information that can be utilized in a number of situations.
The course included lectures, slide presentations, videos, question and answer sessions, and hands-on practical skills application. A training manual and all necessary materials for the course were provided.
The course I attended was taught by Kerry “Pocket Doc” Davis, founder of Dark Angel Medical, and Ross Francis, his chief instructor. Both are outstanding instructors who brought with them a wealth of practical real-world experience and passion for the material they presented.
Direct Action Response Training class was taught by Kerry “Pocket Doc” Davis, founder of Dark Angel Medical (shown here), and Ross Francis, his chief instructor.
Table of Contents
INSTRUCTORS
Kerry Davis joined the U.S. Air Force in 1991 and served until 2007 as an ER medic, flight medic and officer training school instructor. He attended U.S. Army Airborne School at Ft. Benning, Georgia while stationed as a flight medic at Pope Field in Ft. Bragg, North Carolina.
He subsequently worked as a civilian paramedic and completed his RN. He has worked as a critical care and emergency room RN since 2003. Kerry is an avid shooter. He has instructed with Magpul Dynamics and is currently a part-time instructor with SIG Sauer Academy.
Ross Francis is a U.S. Navy combat veteran with multiple deployments to Iraq and Afghanistan as a Navy Corpsman and later as a contractor. He is a nationally registered EMT. Ross has flown with the Air Force Pararescue Jumpers (PJ) and was attached to Marine Force Recon scout sniper units as a Corpsman. He currently works in San Bernardino, California as a paramedic.

DART COURSE
The DART course is quite intensive and covers the following:
- Need for training
- History of emergency care
- Ethics and legality
- Physiological and psychological reactions to environmental stress
- Importance of proper combat mindset
- Basic anatomy and physiology of life-sustaining systems
- H, A, B, Cs—Hemorrhage, Airway, Breathing and Circulation
- Breakdown and usage of Individual Med Kit (IMK) components
- Proper stowage and employment of IMK
- Hands-on application of IMK
- Basic and advanced airway management: treating and monitoring tension pneumothorax, sucking chest wounds, and flail chest
- Airway adjunct device placement: nasopharyngeal airway
- Basic first aid and advanced wound care
- Application of bandages, hemostatic agents, and tourniquets
- Recognition and treatment of various injuries (gunshot, laceration, burn, airway, head, orthopedic, environmental)
- Recognition and treatment of hypovolemic (hemorrhagic) shock
- Moving and positioning victims with various injuries
- Response to active shooter situation
- Proper use of cover and cover vs concealment
- Casualty recovery in active shooter situation
- Mass casualty triage procedure
- Emergency medical dialect/lingo (911 protocol, cooperation with LE, Fire and EMS and first responders)
Although that’s a lot to cover in a two-day course, the material was presented with professionalism and enthusiasm, in an efficient, thorough manner conducive to learning. The instructors clearly not only know their stuff but how to present it in an engaging way that keeps the students focused.
The training was conducted much as one would build a building. The instructors first laid down the foundation then built the structure. The slide presentations and videos, many of them quite graphic, and instructor demonstrations reinforced the instruction and drilled the points in, as did the intensive hands-on training that gave students the opportunity to practice the skills they were taught. Students were encouraged to ask questions throughout the course.
Ross Francis demonstrates use of SAM splint as cervical collar on student. SAM splint is a compact, lightweight, and highly versatile device.
TRAINING DAY 1
We began by covering the need for training, history of emergency care, ethics and legality, and warrior mindset. The right mindset will get you through the toughest situations. We covered combat psychology, the effects of stress and the body alarm response. We learned that the keys to success are long-term potentiation (“train how you bleed”) and staying focused.
We moved on to scene safety, situational awareness, and the Cooper Color Code System. Common factors that can affect situational awareness, such as low-light conditions and environmental factors, were also discussed, as well as the importance of personal protective equipment. Personal safety trumps everything else. The instructors presented options to preserve our safety while still providing patient care. It doesn’t help for the healer to become another patient. Sometimes hard decisions have to be made.
We moved on to basic anatomy and physiology, with the H, A, B, C, D, Es (Hemorrhage, Airway, Breathing, Circulation, “Da Brain” (Neuro), and Expose and Environment) the areas of focus. We learned how to assess a patient and identify and treat the most life-threatening injuries.
Student practices insertion of nasopharyngeal airway (NPA), which can also be employed as expedient oropharyngeal airway (OPA). NPA is employed in situations where an artificial form of airway maintenance is necessary, but it is impossible or inadvisable to use an OPA.
HEMORRHAGE
Early in the course, the instructors began to explain the importance and various types of tourniquets. Roughly 80% of combat deaths and 50% of civilian trauma deaths are attributable to hemorrhage. It’s the most preventable cause of death in compressible injuries. Proper use of tourniquets saves lives. We also learned wound packing and the types and use of hemostatic agents and pressure dressings.
Every student was given a Combat Application Tourniquet (C-A-T) at the beginning of class. At random intervals throughout the course, the instructors would call out “tourniquet” and a specific limb for us to apply it. It became a race to see who could be the first to properly apply the tourniquet to our limb. We also took the tourniquet home with us overnight to practice more with it. Needless to say, we all became quite proficient.
Measuring a nasopharyngeal airway. Prior to insertion, measure it from the ear lobe through to the tip of the nose. Safety pin can be inserted through NPA to mark proper depth of insertion.
AIRWAY & BREATHING
After we dealt with treating massive blood loss, we moved on to the respiratory system. The brain constantly needs oxygen, so it’s vital that we get the patient breathing and oxygenated blood circulating as quickly as possible.
We learned to identify whether or not patients had patent (an open and maintainable airway) breathing. We studied the anatomy of the respiratory system and common airway and breathing injuries that could arise as a result of trauma and how to treat them.
Types and use of artificial airways, artificial respiration, barrier devices, and occlusive dressings (and field expedients) were covered, as well as c-spine precautions, c-spine control, the recovery position, and special considerations.
CIRCULATION
After any massive bleeding has been stopped and the patient’s breathing has been assessed, we need to make certain that blood is circulating throughout the body. The body is a hydraulic machine, and blood is the body’s hydraulic fluid. As emergency caregivers, we must keep as much of the patient’s blood inside the body as possible and ensure it is circulating properly.
We studied the anatomy of the circulatory system and learned how to assess and interpret pulses from various points on the body, skin temperature, color, and capillary refill. The importance of thoroughly reassessing the patient periodically or if the condition deteriorates was stressed.
Student practices wound packing with hemostatic gauze. Goals are to pack wound tightly and down to the bone, occluding the artery and creating focused pressure on the hemorrhage. Wound packing is not used for wounds of head, neck, and torso.
“DA BRAIN,” EXPOSE & ENVIRONMENT
We covered the anatomy and physiology of the neurological system and learned how to assess the Level of Consciousness (LOC). Instructors stressed the importance of constantly reassessing mental status. An altered level of consciousness can be an early indicator of “things going bad.” Any deficit in blood, sugar and oxygen will present in the form of an altered LOC.
The next topic was the last step in the assessment process: to expose the patient to assess for further injuries. You don’t want your patient to die due to your lack of attention to detail. After exposure and assessment, take into account the environment. Cover the patient up and keep them warm.
Student role playing. Every student got the chance to play both patient and emergency caregiver. Instructors assessed and debriefed students on patient assessment and treatment.
INDIVIDUAL MEDICAL KIT
The instructors then went over the Individual Medical Kit (IMK). Many students had purchased Dark Angel Medical’s own kit, the D.A.R.K., and the instructors went over each of the kit’s components and why they were included.
For example, you should always use nitrile, since many people have a latex allergy and can go into anaphylactic shock as a result of contact with latex. Many of the kit’s components have “other capabilities” than their primary purpose, and we were given examples of how they may be used. For those who didn’t purchase the kit, time was spent on putting together one’s own kit.

SPECIFIC INJURIES
We moved on to specific injuries and how to diagnose and treat them. There is no hard and fast rule in trauma. The situation and injury dictate the treatment. Injuries were broken down into three categories: minor, emergent, and environmental injuries.
Minor Injuries
These include:
- Lacerations
- Avulsions
- Contusions
- Abrasions
- Fractures
Emergent Injuries
These are severe, sudden traumatic injuries that can be immediately life threatening. They may be a combination of injuries. Emergent injuries include:
- Gunshot wounds
- Stabbing/impaled objects
- Amputations
- Blast injuries
- Chest trauma, including flail chest and sucking chest
- Wound and tension pneumothorax
- Facial injuries compromising airway
- Eviscerations
- Hypovolemic shock
- Anaphylactic shock
Students had option to purchase Dark Angel Medical D.A.R.K. Trauma Kit (Gen 3) at a discount as part of class. D.A.R.K. is one of the most well-thought-out trauma kits on the market.
TRAINING DAY 2
Environmental injuries, which are often overlooked, were the first topic of discussion. They are easy to prevent but can have serious, immediately life-threatening consequences. They include toxins, heat and cold injuries:
- Poisonous plants
- Snakebites
- Insects
- Carbon monoxide
- Thermal injuries, including heat exhaustion, heatstroke, burns, frostnip, frostbite, and hypothermia
The amount of detail and time spent on each type of injury varied, with the greatest emphasis on traumatic injuries and injuries that could be immediately life threatening. Pediatric and K9 injuries were also discussed.
Rather than memorizing one action for each injury, as taught in many first aid courses, we learned that common treatment modalities can address multiple injuries—a trauma treatment force multiplier. A few different techniques can be utilized in multiple combinations. Once again, this is where the understanding of anatomy and physiology come into play.
With specific injuries out of the way, we moved on to victim movement, victim positioning, cover vs concealment, low-light environments, NBC/HAZMAT operations, triage guidelines, and incidents with more than one victim.
Triage is based on a color-code system:
- Green: Minimal (walking wounded)
- Red: Immediate
- Yellow: Delayed
- Black or Blue: Expectant (nothing can be done to save)
Triage prioritizes treatment. In a tactical environment, colored Chemlights are often used to tag victims. The most important thing to remember is “do the most good for those you can help.”
Direct Action Response Training class is hosted at different locations around the country. Scottsdale Gun Club in Scottsdale, Arizona hosted class author attended.
HANDS-ON TRAINING
Hands-on skill stations were set up in the classroom. We practiced inserting the Nasopharyngeal Airway after measuring its correct length on an airway management training dummy. We practiced applying different types of tourniquets, packing wounds (on wound-packing trainers), and applying direct pressure and pressure bandages.
We also practiced splinting and tying a sling and swathe. The instructors were always there to guide us and answer questions. After we had rotated through all the hands-on skill stations, we felt quite confident in our abilities.
Finally, students were paired up to practice our assessment and treatment skills on each other. We each had the opportunity to play emergency caregiver and victim. The victim or an instructor chose the injury. The instructors evaluated and critiqued our performance. It was an excellent learning process.
Each student who completed the training was awarded a certificate of completion and a cool Dark Angel Medical challenge coin.
Students who successfully completed class were awarded certificate and Dark Angel Medical challenge coin. Students also received a Direct Action Response Training Handbook at beginning of class.
MY THOUGHTS
I have only praise for Dark Angel Medical Direct Action Response Training. It’s an outstanding course. The training you receive is invaluable. The course is hosted at various locations around the country throughout the year. Cost is $400 and worth every dollar. You can add a D.A.R.K. Trauma Kit (Gen 3) for only $135 additional as part of your tuition ($169.99 if purchased separately). To register for a course or for information on hosting one, contact Dark Angel Medical.
D.A.R.K. TRAUMA KIT (Gen 3)
The Dark Angel Medical Direct Action Response Training gives you the skills. The Dark Angel Medical D.A.R.K. (Direct Action Response Kit) Trauma Kit (Gen 3) gives you the tools. To quote the company, “This kit has everything you need and nothing you don’t. Life is hard. Keep your med kit simple.”
Each D.A.R.K. has four main components: a custom MOLLE/PALS-compatible pouch, Combat Application Tourniquet® (C-A-T®), trauma shears, and a vacuum-sealed poly bag that Dark Angel Medical refers to as the “insert.” The D.A.R.K. may also be ordered with the SOF® Tactical Tourniquet-W (SOFTT-W). Rip Shears can be added to the D.A.R.K. as an upgrade, instead of the standard shears.
The D.A.R.K. insert is custom built by Dark Angel Medical “in house” and includes HALO™ chest seals, a nasopharyngeal airway (NPA), QuikClot® Combat Gauze LE or Milspec Combat Gauze™ (depending on D.A.R.K. model), NAR Compressed Gauze, four-inch Israeli Bandage®, polycarbonate eye shield, and a Mylar emergency blanket. ChitoGauze hemostatic gauze may be substituted for the Combat Gauze.
Milspec D.A.R.K. kits include a 14 Gauge ARS Chest Decompression Needle (Chest Dart). Civilian/LE kits do not.
The insert poly bag is 5-mil thick for maximum durability and has quick-tear perforations at each corner. One side of the bag features a zip-style closure so the bag can be resealed and stowed if necessary.
Custom made for Dark Angel by First Spear, LLC, the outer pouch is constructed of 500D NIR nylon and features a cap-style lid with a pull-tab, built-in TQ pouch, PALS webbing on both sides, and a retention strap to secure the trauma shears.
It’s available in four colors: MultiCam, Coyote, Ranger Green, and Black. Measuring only 8x3x2.5 inches, the pouch is roughly the same size as a standard double 30-round magazine pouch.
MSRP for the complete kit (Civ/LE) is $169.99. If you ever have to use your D.A.R.K. to save a life, simply provide official documentation and Dark Angel Medical will send you a replacement kit free of charge.
Essentially if you buy a D.A.R.K., you have a kit for life, which is a pretty good guarantee.
SOURCES
DARK ANGEL MEDICAL, LLC
(720) 836-7150
www.darkangelmedical.com
SCOTTSDALE GUN CLUB
(480) 222-4351
www.scottsdalegunclub.com